As shown in the list of references, quite an amount of research has been published in recent years. It is not possible to cite all of these, therefore the latest publication is summarized, which is added by some important ones that are less recent.
Patty Ku, future IATF member from Taiwan published her MSc-thesis recently in Scientific Reports (2020) about the effects of Ai Chi for balance in individuals with chronic stroke. She compared Ai Chi with conventional aquatic exercise. The intervention lasted for 6 weeks, 3 times per week and 60 minutes per session. Among the test; BBS, Fugl-Meyer assessment (FMA) and (on a force platform) the limits of stability (LOS) were used. BBS and FMA increased in both groups, but significantly more in the Ai Chi group. LOS in anterio-posterior direction only increased in the Ai Chi group. She concluded that Ai Chi is feasible for balance training in stroke and is able to improve shifting in anterio-posterior axis, functional balance and lower extremity control compared to conventional aquatic exercise. See: https://doi.org/10.1038/s41598-020-58098-0
Devereux and co-workers developed an investigation based on Tai Chi exercises adapted to the aquatic environment. 60 The objective of this study was to verify the influence of a hydrotherapy program on balance, fear of falling and quality of life in community dwelling elderly female subjects with a diagnosis of osteopenia or osteoporosis. Participants had an average age of 73.3 years and were randomized to the aquatic group or a control group that continued with their usual activities of daily living. The aquatic group undertook a 10-week program twice a week in 60-minute sessions. The exercises were not described but included a variety of activities including land-based Tai Chi transferred to the water. Devereux observed significant improvements in the experimental group regarding the Step Test (ST), a test that evaluates dynamic balance. Devereux’s results are in accordance with the results obtained in the study by Teixeira et. al.61, in respect to the dynamic balance sub-scale of the Tinetti test. The relative contribution of the aquatic Tai Chi part is unknown however.
A second research report on the use of Ai Chi was published by Ribero Queroz et al.62 They used 9 movements in a series of 10 sessions of 30 minutes with a cohort of Parkinson patients (n = 10) between 50 and 50 years. The Hoehn & Yahr stages were not given. No assessment instruments specific for Parkinson were used. They quantified observations of motor control, using video. The authors concluded that the comparative graphics showed fairly significant changes in postural tremor, dynamic balance, static balance and gait.
Noh et al. used a combination of Halliwick and Ai Chi to increase balance.63 They randomly allocated 25 chronic ambulatory stroke patients (average time of the stroke was 2.2 years) to either an aquatic group or a dry land gym exercise group. Both groups were baseline comparable in terms of gender, age and severity of stroke. Both interventions lasted for 8 weeks, 3 times per week and 60 minutes per session. The Ai Chi part of the aquatic intervention consisted of 20 minutes of two specific movements: Rounding and Balancing. Statistical and clinical significant effects were seen in the Berg Balance Scale (BBS) and in accordance with the results obtained by Teixeira et al, in respect to the static or balance sub-scale of the Tinetti test. Noh et al calculated an effect size of 1.03 in the BBS. Also weight-bearing ability, measured on a force platform showed effect sizes of 1.13 and 0.72 for forward and backward weight-shifting respectively. The authors concluded that aquatic therapy based on Halliwick and Ai Chi improves postural balance.
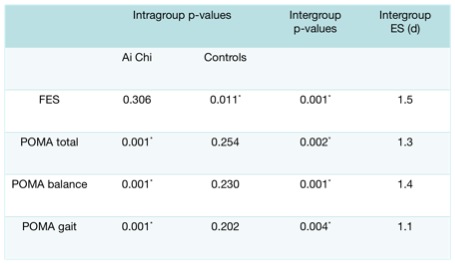
Teixeira et al. performed an assessor blinded randomized trial about the influence of Ai Chi on balance and fear of falling among older adults.61 Home dwelling frail elderly (n = 30), clients of a day care centre were randomly allocated to an Ai Chi class or to a control group receiving usual care. The groups were baseline comparable with an age of 82 ± 2 years and all participants had a medium to high risk of falling (POMA / Tinetti = 14 ± 6). The intervention group received 16 Ai Chi sessions over a period of 6 weeks, according to the sequence suggested by Sova & Konno.2 The POMA was used to evaluate static and dynamic balance and fear of falling was measured with the Falls Efficacy Scale. The time points were pre-intervention and directly post-intervention, but subsequent follow-up did not take place. Results are shown in table 2.This investigation’s findings suggest that an Ai Chi program leads to a clinical relevant increase of both static and dynamic balance in older people, in comparison with usual care. The Ai Chi group remained at the same level of fear of falling, while the participants of the usual care group increased their fear of falling over the research period.